Ways to Avoid Common Medical Coding Errors
Stay Up-to-Date With Coding Changes
Since new codes are added and tweaked annually, best practices for how to code patient diagnostics, encounters, and procedures performed will vary a little bit each year.
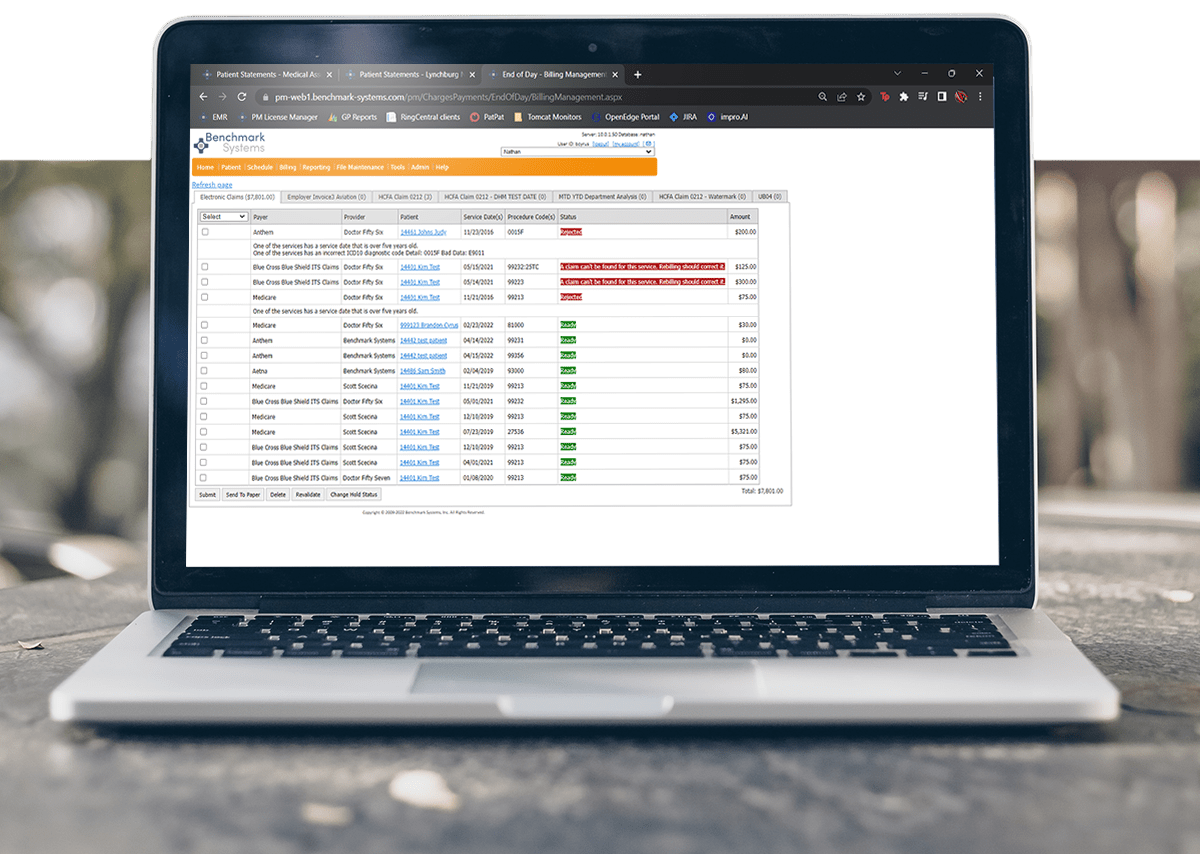
Use an EHR With Built-In Coding Recommendations
EHR coding recommendations reduce medical coding errors and streamline manual data entry. Benchmark EHR offers built-in CPT and ICD-10 code recommendations based on a patient’s medical history or diagnoses, and a user-friendly search function to make finding and inputting the right codes a faster process. Learn more about EHR Coding Recommendations.
Hire Dedicated Billing Specialists
Whether you have an in-house billing team or outsource your revenue cycle management, it’s critical to hire experts who are uniquely qualified and trained to submit claims. For many practices, outsourcing medical billing services can save costs while improving first-pass clean claims rates, increasing collections, and reducing time to AR from an average of 56 days to just 30 days.
Collaborate With Payors
Working with insurers before procedures can help reduce claims denials and improve revenue cycle management. Gaining prior authorizations also benefits patients. They receive fewer surprise bills and have more peace of mind before receiving medical care knowing insurance will cover a portion of the costs. Learn more about how practice management software helps providers manage prior authorizations.