What is medical coding?
Medical coding occurs when a healthcare professional or medical coder translates diagnostic and procedural information into a universal set of alphanumeric codes. These codes correspond with a patient’s diagnosis, treatment, medical necessity, or other procedural information related to the visit. Medical coders examine a patient’s medical record, which includes their doctor’s notes, laboratory tests, diagnostic information, requested imaging studies, and any other relevant sources to verify what services were provided.
The two most common medical coding classifications are the International Classification of Diseases (ICD) and the Current Procedural Terminology (CPT). These codes are entered into an electronic health record system to promote proper medical record keeping and streamlined claims and billing processes.
To prevent medical coding errors, many healthcare organizations rely on electronic health record (EHR) software with built-in coding recommendations or they outsource medical coding, billing, and revenue cycle management services. Proper medical coding avoids insurance payment denials and helps medical practices keep control of their cash flow.

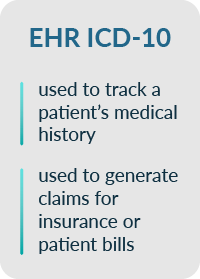 The International Classification of Diseases 10th Revision (ICD-10) was authorized for publication by the World Health Organization in 1999 to help classify diseases and injuries. ICD-10 codes are entered by healthcare personnel or medical coders who assign a code to describe a patient’s diagnosis.
The International Classification of Diseases 10th Revision (ICD-10) was authorized for publication by the World Health Organization in 1999 to help classify diseases and injuries. ICD-10 codes are entered by healthcare personnel or medical coders who assign a code to describe a patient’s diagnosis. 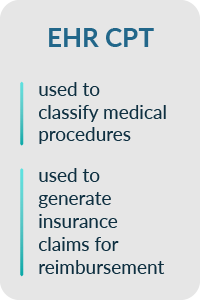 Current Procedural Terminology (CPT) codes are a standardized set of codes used to classify medical procedures. CPT codes are added to a patient’s medical record to track a history of procedures. They are also used to generate insurance claims for reimbursement. On a macro scale, CPT codes may be used by public health professionals to track the incidence of certain medical procedures and monitor healthcare trends. There are currently 10,000 CPT codes in use, according to the American Medical Association, though this number changes on an annual basis.
Current Procedural Terminology (CPT) codes are a standardized set of codes used to classify medical procedures. CPT codes are added to a patient’s medical record to track a history of procedures. They are also used to generate insurance claims for reimbursement. On a macro scale, CPT codes may be used by public health professionals to track the incidence of certain medical procedures and monitor healthcare trends. There are currently 10,000 CPT codes in use, according to the American Medical Association, though this number changes on an annual basis.