Medical practices must carefully document and collect reimbursement for services provided to prevent financial strain. As a result, medical professionals are often tasked with managing the complex process of collecting payments from insurance companies as well as patients themselves. Benchmark Revenue Cycle Management (RCM) is here to share the workload so providers can spend more time with their patients and less time dealing with the practice’s financials.
The Revenue Cycle shown below demonstrates what Benchmark RCM handles for medical practices. We understand not all practices are one size fits all, that why we can tailor any service to the needs of your practice. We will assign a dedicated RCM specialist to your practice to ensure your financials are getting the attention they deserve.
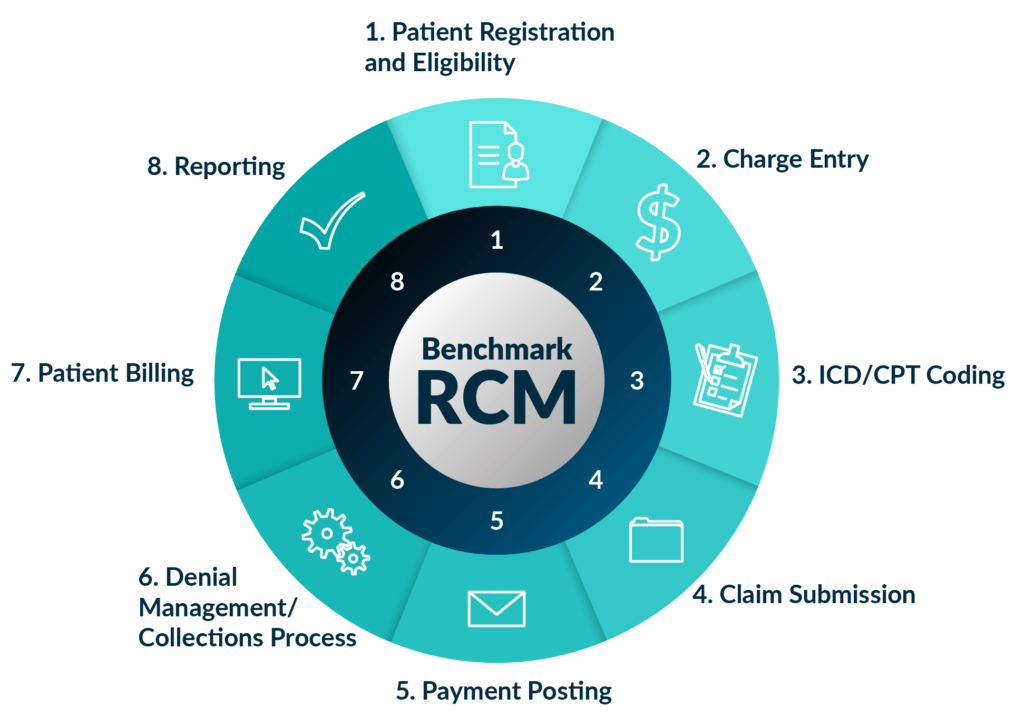
- Patient Registration and Eligibility
Benchmark RCM works to accurately place all demographic and insurance entries into the billing platform. - Charge Entry
Entry of all charges are then billed to insurance and/or patient. - ICD/CPT Coding
Benchmark RCM works to ensure proper diagnosis and procedure code are on claim for payment. Benchmark RCM offers everything from code review up to direct coding from notes. - Claim Submission
Our integrated clearinghouse allows for quick and accurate claims submission and filing. Benchmark RCM has a 98% first pass submission rate. Benchmark RCM offers everything from code review up to direct coding from notes. - Payment Posting
After claims are created and sent to insurances, the practice will receive a Remittance Advice or Explanation of Payment from the insurance carrier in the mail. Practice will then fax or scan to our RCM team for payments to be posted. - Denial Management/Collections Process
If there are any denials, Benchmark RCM works to correct any discrepancies and re-submit to insurance or have an insurance representative reprocess claim. Denials are worked until there is no additional recourse. Our team will work with a collection agency of the practices’ choice and whether to send delinquent accounts to collections. - Patient Billing
Benchmark RCM works to generate patient statements and determine an efficient process for sending patient statements. Benchmark RCM offers Benchmark Pay, an online payment portal that works to receive electronic payments directly from the patient. If the practice decides to send patients to collections, our RCM team works directly with several collection agencies to make information submission seamless. - Reporting
Benchmark RCM works with practices to determine specific reporting requirements and desired reporting schedules. In addition, practices are given full access to the Benchmark Solutions platform to access any reports, any time – all billing methods are 100% transparent.
Interested in Benchmark RCM or want to learn more? Reach out to one of our professionals today.